New York, 1935.
A basement morgue.
Concrete walls. Bare bulbs. The smell of formaldehyde and cigarette smoke hanging so thick in the air it almost felt like a second ceiling.
Dr. Dorothy Hansine Andersen stood over the body of a three-year-old girl whose death certificate read “Celiac Disease”—a polite, clinical label that had become a catch‑all diagnosis for children who couldn’t digest food and slowly starved to death.
But something about this little girl wasn’t right.
Dorothy had seen “Celiac disease” before. She knew the pattern. Fragile kids, struggling to gain weight, wasting away slowly. Yet these children in her morgue had a different story written into their bodies.
They ate ravenously. They weren’t refusing food. They consumed everything in sight—like their bodies were begging for nutrients. And still, they withered away, their bellies swollen and round, their arms and legs frighteningly thin.
And the lungs—always the lungs.
When Dorothy opened their chests, she found airways clogged with thick, sticky mucus. Heavy, viscous, suffocating. It coated their lungs, filled the spaces where breath was supposed to live.
Celiac disease didn’t do that.
Something else was killing these children.
The Surgeon She Wasn’t Allowed to Be
Dorothy Andersen had not planned to spend her life in a basement with the dead.
She’d graduated from Johns Hopkins Medical School in 1926—one of the best programs in the world. She was brilliant, driven, and unapologetically ambitious. She wanted to be a surgeon.
She wanted the bright lights of the operating room.
She wanted to hold living hearts in her hands and fix what was broken.
She applied for a surgical residency.
On paper, she had everything:
The grades. The recommendations. The talent. The stamina.
But in 1920s America, she lacked something the gatekeepers considered non‑negotiable.
She was a woman.
Surgery, they said, was for men. Men did bold, decisive things. Men made life‑or‑death calls. Men took charge. Women, if they were allowed in medicine at all, could assist. Observe. Stay in the background. Or, better yet, study the dead.
The rejection wasn’t subtle. They didn’t even bother to dress it up. It wasn’t about her intelligence. It wasn’t about skill. It was about gender—nothing more, nothing less.
So they pushed her into pathology.
The message was clear:
You want to cut? Fine. You can cut the dead.
The Woman the Basement Didn’t Break
Dorothy could have accepted the insult and quietly faded into a safe, unremarkable career. But that wasn’t who she was.
She wore hiking boots instead of heels.
She chain‑smoked through autopsies, a cigarette often hanging from the corner of her mouth as she leaned over a body.
She built her own furniture. She hosted rowdy parties in her lab. She laughed loudly. She swore. She didn’t shrink herself to fit the room.
If the medical establishment wanted her to disappear into the basement, she would do the opposite.
She would take up space.
She would make noise.
She would turn the morgue into a front line.
So when she found herself surrounded by tiny bodies with the same maddening, unexplained pattern—ravenous hunger, starvation, distended bellies, sticky lungs—she made a private decision:
If they wouldn’t let her save lives in the operating room, she would save them from the morgue.
The First Cut That Changed Everything
Back in that cold, fluorescent basement, she opened the three‑year‑old’s abdomen with methodical precision. Her hands were steady. Her mind was anything but calm.
She reached for the pancreas.
It should have been soft and smooth. In a healthy child, the pancreas is an unremarkable organ, quietly producing enzymes that help digest fat, protein, and carbohydrates.
What she saw instead looked like an organ that had been attacked.
The pancreas was riddled with cysts. Scar tissue twisted through it like vines. The ducts—the tiny pathways that were supposed to carry digestive enzymes into the intestines—were blocked completely, clogged with material that had no business being there.
This child had not died of Celiac disease.
She had starved from the inside out.
Her stomach had been full. Her appetite had been strong. But her organs had betrayed her. No matter how much food passed through her mouth, none of it truly reached her body.
And in that moment, staring at the destroyed pancreas of a three‑year‑old, Dorothy understood something chilling:
This wasn’t an isolated tragedy.
This was a pattern.
A Hidden Killer in the Files
She went to the records.
She pulled files on nearly 50 children who’d died with “Celiac disease” listed on their death certificates. The ones nobody questioned. The ones doctors shrugged over with a sad, clinical inevitability: “some children just die.”
Night after night, Dorothy sat alone with stacks of autopsy reports and slides. She cross‑referenced findings. She reread descriptions of lungs, pancreases, intestines. She traced the same injuries, the same scars, the same strange mucus.
There it was.
Over and over again:
The scarred pancreas.
The blocked ducts.
The mucus‑filled lungs.
Not in a handful of cases. In case after case.
This was not Celiac disease.
This was something else entirely—a distinct disease hiding in plain sight, slipping through the cracks while doctors blamed the wrong culprit.
She gave it a name:
“Cystic Fibrosis of the Pancreas.”
At the time, it probably felt almost small—a technical term, a label pinned onto a terrifying mystery. But names matter. You cannot fight what you cannot name.
And Dorothy had just named an invisible killer.
Finding the Living Before They Reached Her Table
But identifying the enemy was only the beginning.
Children weren’t just dying in her morgue. They were dying on pediatric wards across the country, misdiagnosed and treated for the wrong disease. They were wasting away while parents begged for answers and doctors repeated an old, familiar story:
“It’s Celiac. There’s nothing more we can do.”
Dorothy knew better now. But knowing wasn’t enough. She needed a way to separate the children with Cystic Fibrosis from those with genuine Celiac disease—while they were still alive.
So she did what good scientists do:
She built a test from scratch.
She developed a diagnostic procedure that involved extracting fluid from the duodenum, the upper part of the small intestine. A tube had to be passed down the child’s throat, through the stomach, into the duodenum, where the pancreatic enzymes could be measured.
It was invasive. Uncomfortable. Not the kind of test anyone wanted to put a child through unless absolutely necessary.
But it worked.
For the first time, doctors had a way to distinguish Cystic Fibrosis from Celiac disease. For the first time, they could say:
“This isn’t what we thought it was. This child has something else—and we can treat it differently.”
For the first time, some of those children had a chance to be treated as patients, not puzzles.
And Dorothy wasn’t finished.
The Heat Wave Clue
In the brutal summer of 1948, New York City sweltered under a wave of punishing heat. Temperatures soared. Streets shimmered. Hospitals filled with people collapsing from exhaustion and dehydration.
In the pediatric wards, Dorothy noticed something alarming.
Children with Cystic Fibrosis seemed to be collapsing at an unusually high rate. Not just one or two. Many of them. They came in listless, weak, dangerously dehydrated.
Why these kids? Why now?
She and Dr. Paul di Sant’Agnese began digging. They considered the obvious: lungs, digestion, infection. But nothing explained the pattern. Then they looked at something most people ignored:
Sweat.
CF patients, they realized, were losing massive amounts of salt through their sweat—far more than healthy children. Their bodies were literally leaking sodium and chloride, turning a heat wave into a lethal threat.
From that insight came something revolutionary in its simplicity:
the “sweat test.”
Instead of threading tubes into intestines, doctors could stimulate sweat on a child’s skin, collect it, and measure the salt content. High chloride levels pointed strongly toward Cystic Fibrosis.
Non‑invasive.
Relatively painless.
Repeatable.
Dorothy’s work, combined with di Sant’Agnese’s, turned a mysterious, deadly illness into something doctors could reliably detect.
Today, more than 75 years later, the sweat test is still the gold standard for diagnosing Cystic Fibrosis.
What began in a basement morgue had turned into a clinical tool used in hospitals worldwide.
The Paper That Changed Pediatric Medicine
In 1938, Dorothy Andersen published the landmark paper that changed everything.
It wasn’t just a case report. It was an atlas of a disease no one had properly seen before. She described the pathology in painstaking detail—the scars in the pancreas, the mucus in the lungs, the damage in the digestive system.
She drew clear distinctions between Cystic Fibrosis and Celiac disease. She laid out diagnostic criteria. She outlined how to recognize these children before it was too late.
She didn’t stop at describing. She helped pioneer early enzyme replacement therapies that allowed CF patients to actually digest their food. Suddenly, children who had been written off as doomed “malabsorption” cases had a shot at growth, at gaining weight, at living longer.
In the 1930s, most children with Cystic Fibrosis died before their first birthday. Many didn’t make it past toddlerhood.
Dorothy’s work didn’t cure the disease. That would take decades more research and countless other scientists building on her foundation. But she was the one who dragged CF out of the shadows and into the light.
She gave it a name.
She gave doctors a map.
She gave families something they’d never had before:
an explanation—and hope.
The Rebel in Hiking Boots
Outside the pages of medical journals, Dorothy Andersen refused to become the quiet, soft‑spoken woman the world expected.
She never married. She climbed mountains. She spent her free time hiking, building, fixing things with her own hands. She was not interested in playing a role to make others comfortable.
In an era when women were expected to be demure and accommodating, she was rugged, blunt, and unapologetically herself.
Colleagues remembered her in hiking boots and practical clothes, cigarette smoke framing her face as she cut through a post‑mortem like a seasoned mechanic dissecting an engine. She was intimidating to some, inspiring to others.
She didn’t just work with the dead. She trained the living.
She taught cardiac surgeons how to repair the hearts she’d studied in the morgue, translating her pathological findings into surgical strategies. She turned autopsy rooms into classrooms, connecting what she saw in still organs to what could be done in a beating chest.
She proved, over and over again, that the medical establishment’s refusal to let her into surgery had not diminished her impact there. It had simply changed the angle.
They wouldn’t let her stand at the operating table.
So she stood behind it and made the work better anyway.
Refusing to Accept “Some Children Just Die”
Maybe her greatest legacy isn’t one test or one paper. It’s the attitude she carried into that basement every single day.
At the time, it was common—almost accepted—for children’s deaths to be written off with vague diagnoses and shrugged shoulders. “Celiac disease.” “Failure to thrive.” “Unknown causes.”
To many, this was just the tragic reality of pediatrics.
But when Dorothy saw a pattern that didn’t fit the textbooks, she didn’t accept it. When a label didn’t match the evidence carved into the bodies on her table, she didn’t defer to authority.
She trusted her own eyes.
She trusted what the bodies were telling her.
When doctors wrote “Celiac disease” on death certificates without proof, she said:
No. Find the real answer.
When the medical establishment told her women had no place in surgery, she said:
Fine. I’ll build a different kind of scalpel.
When the system tried to bury her in a basement, she treated that basement like a war room.
The Revolution from the Morgue
By the time she died of lung cancer in 1963—ironically, the chain‑smoking pathologist claimed by the very organ she’d spent her life studying—Dorothy Andersen had helped shift the trajectory of an entire disease.
Children with Cystic Fibrosis now live into their 40s, 50s, and beyond.
There are targeted treatments, specialized clinics, and new therapies that would have been unimaginable in the 1930s.
None of that happened by accident. It happened because one woman, denied the career she wanted, refused to waste the one she was given.
She was relegated to the basement.
She changed medicine from there.
Dorothy Hansine Andersen (May 15, 1901 – March 3, 1963):
The woman told she couldn’t be a surgeon because of her gender.
The pathologist who studied dead children to save the living.
The chain‑smoking, boot‑wearing rebel who mapped an invisible killer and gave thousands of children a chance at life.
She was never supposed to be a revolutionary. She was supposed to be a footnote—a woman quietly tucked into a “suitable” medical specialty.
Instead, she turned the cold, silent world of the morgue into a place where the dead spoke, and she listened.
That’s not just a career.
That’s a revolution.
News
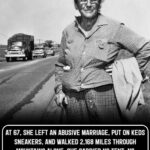
Emma Rowena Gatewood was sixty‑seven years old, weighed about 150 pounds, and wore a size 8 shoe the day she walked out of the ordinary world and into the wilderness.
On paper, she looked like anyone’s grandmother. In reality, she was about to change hiking history forever. It was 1955….
21 Years Old, Stuck in a Lonely Weather Station – and She Accidentally Saved Tens of Thousands of Allied Soldiers
Three days before D‑Day, a 21‑year‑old Irish woman walked down a damp, wind‑bitten corridor and did something she’d already done…
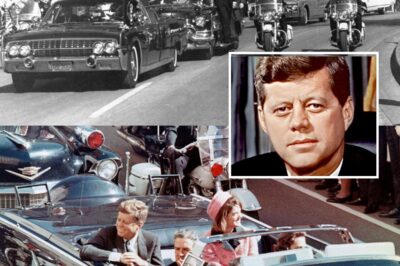
JFK’s Assassination Was Way Worse Than You Thought
So, he’s finally done it. What do these new documents tell us about that fateful day in Dallas? In 2025,…
US Navy USS Saufley DD465 1952 Living Conditions
The USS Southerly was a general‑purpose 2,100‑ton destroyer of the Fletcher class. She was originally equipped to provide anti‑aircraft, surface,…
Man Finds Birth Mother and Uncovers His Family’s Unbelievable Past
Air Force Colonel Bruce Hollywood always knew he’d been adopted. His Asian features clearly didn’t come from his parents, who…
Before the wedding began the bride overheard the groom’s confession and her revenge stunned everyone
The bride heard the groom’s confession minutes before the wedding. Her revenge surprised everyone. Valentina Miller felt her legs trembling…
End of content
No more pages to load