Toronto General Hospital, January 1922.
The windows were filmed with frost. The corridors were long and cold, smelling of disinfectant, gauze, and a kind of quiet despair that clung to the walls.
On a narrow iron bed in one of the “no-hope” wards, a boy was slowly fading out of the world.
Leonard Thompson.
Fourteen years old.
Barely 65 pounds.
His skin was pale and tight over his bones. His eyes were sunken deep into their sockets. Each breath he took carried a faint, sharp smell—like nail polish remover.
Acetone.
A sign that his body had begun to devour itself to stay alive.
Leonard drifted in and out of consciousness. At one moment he opened his eyes and tried to muster a weak smile for his father. A moment later, he slipped back into the dark, his breathing shallow and thin.
Three years earlier, Leonard had been diagnosed with Type 1 diabetes.
In 1919, that diagnosis wasn’t just bad news.
It was a death sentence.
There were no insulin injections.
No insulin pumps.
No blood glucose meters.
There was only one answer doctors could give:
Your child is going to die.
The “treatment” that starved children to buy them time
At that time, medicine had exactly one response to Type 1 diabetes:
They called it “careful dietary regulation.” It sounded scientific. It sounded responsible.
In reality, it was controlled starvation.
If sugar was killing the patient, the logic went, then the only option was to remove as much sugar-producing food as possible.
Not just reduce it. Strip it down to the bare minimum.
Leonard was restricted to fewer than 450 calories a day.
Less than what a toddler might eat.
Less than two small meals.
His meals were weighed out on scales. Measured in grams. No bread. No sweets. Almost no carbohydrates. Very little fat. Just enough to stop him from dying immediately.
His parents, Harry and Leonard’s mother, watched their son shrink in front of them. Trousers that used to fit now slipped from his waist. Round cheeks hollowed into the sharp, gaunt face of someone who looked decades older than he was.
The cruelest part?
They knew this was “the best” medicine could offer.
Do nothing, and he would die quickly from diabetic complications.
Follow the starvation diet, and he would die slowly from malnutrition.
Two paths.
Both led to the cemetery.
Many children didn’t make it a year. Some held on a little longer. But all of them were heading toward the same end.
By late 1921, Leonard was reaching that end.
His blood sugar was wildly out of control. He was too weak to sit up on his own. His breathing was rapid and labored. Doctors knew: he was in the final phase.
The Thompson family brought Leonard to Toronto General Hospital.
It wasn’t really a treatment trip.
It was a farewell.
The doctors were brutally honest with Harry:
Your son is dying.
There is nothing in conventional medicine that can save him.
But there was something outside the boundaries of conventional medicine.
Something experimental.
Something that had never been tried in a human being.
The “average” doctor with a theory no one really believed
While Leonard lay suspended between life and death, a young Canadian surgeon named Frederick Banting was spending his nights in a cramped, makeshift laboratory at the University of Toronto.
Banting was not a prodigy in the usual heroic mold. He wasn’t top of his class. He wasn’t a famous name. His private practice had failed. He lived modestly, without much to distinguish him—except for one thing:
He was stubborn.
Almost aggressively stubborn.
And he had become obsessed with one organ: the pancreas.
From prior research, he believed the pancreas produced a vital internal secretion that controlled blood sugar. If that secretion could be isolated, he thought, perhaps diabetes could be treated.
Many scientists had suspected something similar before. But they hadn’t gotten far enough to turn theory into therapy.
Banting decided he’d go further.
He brought his idea to Professor John Macleod, an established expert on carbohydrate metabolism.
Macleod listened, unimpressed. The idea seemed crude, naive, overly simplistic. But eventually—perhaps out of curiosity, perhaps thinking nothing would come of it—he agreed to give Banting the bare minimum:
A small lab.
Several dogs.
And a medical student named Charles Best to help.
That was it.
Enough to fail quietly—or to change medicine forever.
A summer of dogs, scalpels, and “thick brown muck”
In the summer of 1921, while life went on outside—people working, families picnicking, couples courting—two men in a hot, airless lab were cutting into dogs and measuring sugar.
Banting and Best removed the pancreases from some dogs, inducing diabetes artificially. Their blood sugar shot up. They lost weight rapidly. They became listless and sick—mirror images of the children with diabetes outside the lab.
Then they took pancreases from other animals, ground them up, and used alcohol to extract the internal secretion.
What they produced was a cloudy, thick brown liquid.
Hardly the stuff of medical miracles.
Colleagues looked at the viscous extract and scoffed:
“That? You’re never going to inject that into a human being.”
Banting and Best weren’t laughing. They injected it into their diabetic dogs.
And then they saw it:
The animals’ blood sugar dropped.
Their condition improved.
Dogs on the brink of death began to recover.
Not once. Repeatedly.
With every successful experiment, the “crazy” idea looked less crazy and more like a real discovery.
But one major obstacle remained:
You cannot inject “thick brown muck” into people.
The extract needed to be purified.
Enter James Collip, a biochemist Macleod recruited to join the team. His job was to do what Banting and Best could not: transform their crude extract into something clean and consistent enough to inject into a human being.
By January 1922, working together—Banting and Best with their dog experiments, Collip with his purification methods, and Macleod overseeing and guiding—they had a preparation they believed might be ready.
Now they needed something science alone could not supply:
A real patient.
On the brink of death.
With a family desperate enough to say yes.
A father forced into a choice no parent ever wants
Leonard Thompson was that patient.
He had nothing left to lose.
More accurately: he was about to lose everything.
His body was failing. His blood sugar was lethal. His organs were under siege. He was at the edge.
The doctors at Toronto General told the Thompsons about the experimental pancreatic extract.
There was no comfort in the way they presented it:
No promise.
No safety data.
No prior human cases to point to.
Only this:
“We have something that might help. Or it might not.
We’ve never used it on a person.
We cannot promise anything.”
To most people, that would sound terrifying.
Too dangerous. Too uncertain.
But when your child is already dying, “danger” looks very different.
Harry Thompson had to look at his son on that hospital bed—emaciated, barely conscious—and decide whether to allow strangers to inject an unknown substance into him.
This wasn’t a choice between safe and unsafe.
It was a choice between certain death… and a gamble.
He chose to gamble.
He chose hope.
Even if hope, at that moment, looked a lot like a last desperate throw of the dice.
The first injection: failure, and a cold slap of reality
January 11, 1922.
In Leonard’s hospital room, doctors prepared the syringe.
Inside was the first batch of pancreatic extract purified enough, in theory, to be injected into a human.
No monitors.
No glucose meters.
No IV pumps.
Just a syringe, a stethoscope, and a handful of men whose faith in their work had to fill in the vast gaps in knowledge.
The needle went in. They injected the extract.
Then they waited.
If this was going to be a miracle, the first signs would show up soon.
If it was going to be a disaster, they would see that too.
It was neither.
Leonard developed hives—a clear allergic reaction. The extract was still too impure, contaminated with proteins and other substances that his body rejected. His blood sugar barely moved.
No obvious improvement.
No sudden clarity or strength.
Just a sick boy, now with a reaction to whatever they had just given him.
The team could have stopped there.
They could have concluded that the treatment was too dangerous, or that it wouldn’t translate from dogs to humans. They could have written their failure up in a journal and walked away.
They didn’t.
Twelve days of life-or-death waiting—and a lab that never slept
After the failed first injection, James Collip went back to the laboratory and almost didn’t leave.
He pushed deeper into the chemistry of the extract.
He tweaked alcohol concentrations, refined his filtration steps, removed more and more impurities. He worked as if there were a literal countdown clock in his head.
There was.
It was called Leonard Thompson.
In the hospital, Leonard continued to weaken. His father watched helplessly as his son drifted closer to the edge. Each day felt longer, heavier. Each night, more uncertain.
Twelve days.
Twelve nights.
Twelve rounds of: “Will we be too late?”
For Leonard’s family, those days were pure suspension—hanging between hope and grief.
For Banting, Best, Collip, and Macleod, they were a test:
Could they turn a fragile, one-off lab result into something reliable enough to challenge death itself?
The second injection: the moment history turned
January 23, 1922.
Once again, doctors walked into Leonard’s room with a syringe in hand.
This time, the liquid inside was clearer, purer, refined by twelve days of relentless biochemical work.
They injected Leonard.
There were no crowds. No cameras. No speeches.
Just a thin boy on a bed, a worried father, and a handful of men silently willing reality to bend.
Then, slowly, the numbers told the story.
Leonard’s blood glucose began to fall—from dangerously high levels down toward normal.
The toxic acids in his body decreased.
The acetone smell on his breath began to fade.
He woke up more alert. His eyes were brighter.
He said he felt stronger.
His medical notes would later record:
“The boy became brighter, more active, looked better and said he felt stronger.”
This wasn’t a miracle in the mystical sense.
It was chemistry.
It was physiology.
But to anyone watching, it felt like a boy being pulled back from the grave.
Leonard received daily injections through early February. He began to gain weight. His cheeks filled out. He could sit up. He could move.
In May 1922, Leonard Thompson left Toronto General Hospital.
Not in a coffin.
On his own two feet.
The story escapes the hospital—and the world explodes
In an age before social media, big news traveled slower—but it still traveled fast.
A boy with terminal diabetes had been brought back from the edge by injections of a pancreatic extract.
A disease that had always been a guaranteed death sentence now seemed… treatable.
Newspapers rushed to cover the story.
The New York Times declared:
“One by one the implacable enemies of man are overcome by science. Diabetes is the latest to succumb.”
The press hailed a “Toronto miracle.”
Doctors wrote from around the world asking for details, recipes, protocols.
Most importantly, parents began writing too.
And they didn’t write like scientists.
They wrote like people standing in deep water, reaching for the last piece of driftwood.
A blizzard of desperate letters: “My child is dying. Please send insulin.”
As the news spread, the University of Toronto was overwhelmed with letters.
“My wife is dying of diabetes. Please send the serum.”
“My little boy has only weeks left. We read about Leonard. Please, we are begging you.”
“My daughter is wasting away. Can you send some of the extract? We will pay anything.”
They weren’t asking for a miracle.
They were asking for a chance.
But the lab in Toronto was not a factory.
Banting, Best, Collip, and Macleod could make enough for a handful of patients. Not hundreds. Not thousands.
Worse, between March and May 1922, Collip struggled to reproduce his purification process at scale. Production stalled completely.
For a period of time, insulin—this new lifeline—was available in fits and starts. Leonard himself went through stretches with limited supply, relying on careful diet again when insulin ran out.
Once more, he became a symbol of transition:
Living in the gap between a world with no hope and a world not yet able to deliver hope reliably.
That gap needed something only industry could provide.
When science needed factories
By mid-1922, Eli Lilly and Company, a pharmaceutical manufacturer in the United States, entered the picture.
The University of Toronto partnered with Lilly to scale up insulin production.
Their goal: turn a fragile, hand-crafted lab process into a robust industrial operation—pure, consistent, and high-volume.
Chemists, engineers, and factory workers joined the effort.
Insulin began to be produced from animal pancreases on an industrial scale.
By 1923, insulin was being shipped across North America and then to other parts of the world.
Children who would have died on starvation diets started gaining weight instead of losing it.
Adults once resigned to a short life began working, planning, marrying.
Leonard had been the first.
But after him came a tidal wave of lives reclaimed.
Twenty-one months to a Nobel—and a quiet act of defiance
In October 1923, barely 21 months after that second injection into Leonard’s arm, the Nobel Committee awarded the Prize in Physiology or Medicine to Frederick Banting and John Macleod.
Twenty-one months.
The shortest interval in history between a medical breakthrough and a Nobel Prize.
The world applauded.
Textbooks etched their names in ink.
But inside the team, the reality was messier.
Banting was enraged that Charles Best—the student who had spent that brutal summer of 1921 working side-by-side with him, day and night—had been left out.
Macleod, who had been cautious at first but ultimately provided critical support, infrastructure, and credibility, was honored alongside Banting.
Immediately, Banting announced he would share half of his Nobel prize money with Best.
Macleod, in turn, shared his half with Collip.
It wasn’t just generosity.
It was an honest correction.
A way of saying:
This was never the work of one genius alone.
It belonged to the whole group:
– The persistent surgeon (Banting)
– The tireless student (Best)
– The rigorous biochemist (Collip)
– The skeptical-but-essential senior scientist (Macleod)
And, indirectly, to one more person:
A fourteen-year-old boy who had risked being the first.
Leonard Thompson: from death sentence to 13 borrowed years
Insulin did not cure diabetes.
It did not erase the diagnosis.
What it did was something quieter but just as radical:
It shifted Type 1 diabetes from “always fatal, quickly” to “chronic and manageable.”
For Leonard, that shift meant this:
Instead of dying in January 1922 at age 14 in a hospital bed, he lived another 13 years.
He put on weight.
He grew up.
He lived a teenage life and young adulthood that, before him, no one with Type 1 diabetes had.
He didn’t become a celebrity.
He didn’t tour the world telling his story.
He simply lived—modestly, quietly, like so many others would come to do.
And that, in itself, was the miracle:
To move from inevitable death to “ordinary”.
On April 20, 1935, Leonard Thompson died of pneumonia at age 27—likely made more dangerous by his diabetes, but not directly from uncontrolled diabetic coma.
Insulin had given him 13 years.
Thirteen birthdays.
Thirteen Christmases.
Thirteen years of memories his parents had never dared hope for.
Without insulin, Leonard would have died in January 1922 at 14.
With insulin, he made it nearly to 30.
A legacy written not in stone, but in syringes and sensors
More than a century after that first successful injection, it’s hard to fully imagine the “before insulin” era.
Today, people with Type 1 diabetes:
– Use insulin pens and pumps.
– Wear continuous glucose monitors.
– Calculate carbs.
– Go to school, to work, to college.
– Fall in love, have families, grow old.
It’s still hard. It’s still demanding.
But it’s no longer automatically fatal.
Every time someone checks their blood sugar, every time someone doses insulin before a meal, they are quietly participating in a story that began in that hospital room in Toronto.
A story that runs straight through:
– Leonard’s sallow, half-conscious body on a narrow bed
– His father’s trembling consent to an untested treatment
– Banting’s and Best’s long nights with diabetic dogs
– Collip’s countless extractions
– Macleod’s reluctant but crucial support
Leonard’s legacy isn’t found in statues or grand monuments.
It’s in:
– Every child with Type 1 whose parents don’t have to plan a funeral.
– Every teenager annoyed at their pump but still alive to be annoyed.
– Every adult living, working, raising children with diabetes instead of dying from it.
What Leonard Thompson really gave the world
Scientists are credited with discoveries.
Companies are credited with production.
But Leonard?
He is often mentioned in a single line: “the first patient to receive insulin.”
It sounds small. But without that single line, the rest of the story might have taken years—maybe decades—longer to unfold.
Without a first human case:
– There’s no proof beyond animals.
– There’s no headline to jolt the medical community awake.
– There’s no emotional momentum pushing industry and hospitals to move faster.
Leonard Thompson was the bridge between two worlds:
– One where Type 1 diabetes was an automatic death sentence.
– And one where it became a disease people live with, not die from immediately.
He was not a scientist, not a doctor, not a professor.
He was a sick child with no options left.
And that placed him in the one position that moves history forward more often than we like to admit:
He was desperate enough to say yes.
When someone today scans their CGM, injects insulin, and goes about their day, they’re walking a path that runs over the place Leonard once lay, waiting to die.
One injection. One boy. One impossible choice.
If you had to freeze this entire story into a single scene, it might be this:
A cold hospital room in early 1922.
A skeletal teenager lying motionless on a bed.
A father standing by, knowing with terrifying clarity that his son is about to die.
And a handful of doctors holding a syringe filled with something no one has ever dared inject into a human being.
They did not know what would happen.
They only knew what would happen if they did nothing.
So they tried.
In doing so, they didn’t just save Leonard for a time.
They punctured a wall that had stood for thousands of years—between humanity and a disease that had always won.
The story of Leonard Thompson reminds us of an uncomfortable but vital truth:
Progress rarely comes from certainty.
It comes from:
– Parents refusing to accept “there’s nothing more we can do.”
– Scientists refusing to stop after the first failure.
– Patients and families willing to be first, even when “first” might also mean “sacrifice.”
Leonard Thompson was the first person to receive insulin and live.
The first proof that insulin therapy could work in human beings.
The first sign that diabetes didn’t have to be a death sentence.
Because he went first, millions didn’t have to.
That isn’t just a medical milestone.
It’s a revolution—
born in a cramped lab, a cold hospital room, a single syringe…
and the courage of a 14-year-old boy who had every reason to give up, but didn’t.
News
Emma Rowena Gatewood was sixty‑seven years old, weighed about 150 pounds, and wore a size 8 shoe the day she walked out of the ordinary world and into the wilderness.
On paper, she looked like anyone’s grandmother. In reality, she was about to change hiking history forever. It was 1955….
21 Years Old, Stuck in a Lonely Weather Station – and She Accidentally Saved Tens of Thousands of Allied Soldiers
Three days before D‑Day, a 21‑year‑old Irish woman walked down a damp, wind‑bitten corridor and did something she’d already done…
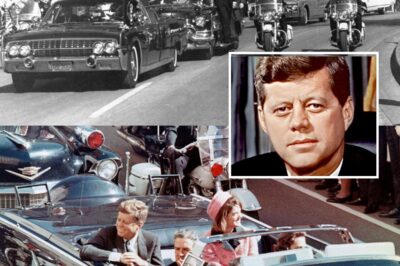
JFK’s Assassination Was Way Worse Than You Thought
So, he’s finally done it. What do these new documents tell us about that fateful day in Dallas? In 2025,…
US Navy USS Saufley DD465 1952 Living Conditions
The USS Southerly was a general‑purpose 2,100‑ton destroyer of the Fletcher class. She was originally equipped to provide anti‑aircraft, surface,…
Man Finds Birth Mother and Uncovers His Family’s Unbelievable Past
Air Force Colonel Bruce Hollywood always knew he’d been adopted. His Asian features clearly didn’t come from his parents, who…
Before the wedding began the bride overheard the groom’s confession and her revenge stunned everyone
The bride heard the groom’s confession minutes before the wedding. Her revenge surprised everyone. Valentina Miller felt her legs trembling…
End of content
No more pages to load